Spring 2014Marriage Before Engagement
A stronger and more nimble marriage between healthcare and the EHR is needed for better patient engagement
by Vikram Kumar MD FAAP, CMIO & Pediatrician, Arrowhead Regional Medical Center
This article conveys opinions of the author, and does not reflect perspectives of the author’s employer or other affiliates.
#patient, #patientengagement, #HIE, #EHR, #patientsatisfaction, #HITECH, #MeaningfulUse, #UI, #TripleAim, #enduser, #clinician, #healthcare
Let’s start at the end. The goal is improved patient health. There are different methodologies that healthcare organizations utilize to improve patient outcomes. These include:
- Improving the quality of patient-care
- Utilizing evidence based medicine practices
- Adhering strictly to compliance and regulatory requirements
- Patient or Family centered medical care
- Addressing patient satisfaction
- Team based systems of care
- Allowing for exchange of medical records between healthcare providers
- Maintaining patient privacy
- Participation in a Health Information Exchange (HIE)
All of these call for increasing patient engagement.
Implementation of an Electronic Health Record (EHR) system is critical to achieve most, if not all, of these goals.
The earliest Electronic Health Records (EHR) were developed in the 1960s as simple data entry and repository systems1. Through the 1970s-1990s, EHRs continued to evolve but were not widely embraced. They were cumbersome to use and often needed significant software and hardware investments.
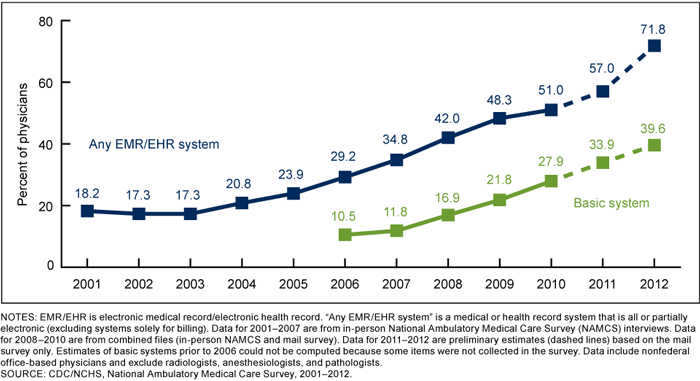
In April 2004, President George W. Bush issued an executive order to provide federal leadership in the development and national implementation of an interoperable electronic patient records system by 20142. Congress enacted the HITECH Act as part of the American Recovery and Reinvestment Act on February 17, 2009. The HITECH Act calls for the voluntary adoption of HIT technology throughout the health care system. The new law substantially expanded the federal government's effort to establish a national electronic patient records system by 2014, while providing for comprehensive records privacy and security standards. The Medicare and Medicaid EHR Incentive Programs provide financial incentives for the “meaningful use” of certified EHR technology to improve patient care. To receive an EHR incentive payment, providers have to show that they are “meaningfully using” their EHRs by meeting thresholds for a number of objectives. CMS has established the objectives for “meaningful use” that eligible professionals, eligible hospitals, and critical access hospitals (CAHs) must meet in order to receive an incentive payment. The adoption of EHRs has increased significantly to a majority of practices and healthcare organizations.3
Figure 1: EHR adoption percentage by year
How happy are the end-users of EHRs?
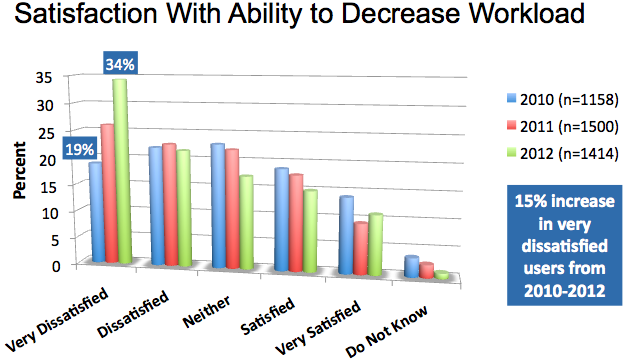
Users of EHR include providers such as clinicians, nurses, assistants and other healthcare workers. In a 2012 survey of clinicians by the American College of Physicians and AmericanEHR Partners user satisfaction decreased by 12 % from 2010 to 20124. In addition about 10 % indicated severe dissatisfaction. This is not an isolated study. Several studies have pointed towards decreased productivities and satisfaction rates amongst EHR users.
Figure 2: EHR Clinician Satisfaction4
EHRs are, in general, wonderful tools to improve patient care. They allow efficient and secure sharing of patient information. They allow real-time transmittal of orders and legible documentation of encounters. And yes, there is no limit to the amount of data that they can hold and that data can be mined for all sorts of information.
The next time you see your doctor; ask her/him how satisfying the EHR rollout has been? Some users are completely satisfied with their EHR, many aren’t5. Every advantage has an equal and opposite disadvantage. Though no EHR end-user will ever want to go back to a paper world, they often complain of the inefficiencies of the EHR.
It is unfair to paint all EHRs with the same brush strokes. Some EHRs do a better job with improving efficiencies and productivities. Others continue to be clunky. Some need multiple clicks or keystrokes. There is also wide variation with the user interface (UI), user customization, electronic workflow and such. The variations with workflow may be at a user, facility or EHR level. It could be something minor such as login time-outs (10 minutes vs. 20 minutes) or something more complex such as template utilization vs. voice-recognized dictations. Hardware and network issues may further cloud the picture.
What is Patient Engagement?
According to the US Department of Health and Human services “The engagement of patients and their families in patients’ health care is a prominent goal of the EHR Incentive Program (also called Meaningful Use).6
Patient or Family Engagement includes (and is not limited to)
- Allowing patients and their families access to their medical information (handouts, electronic handouts, patient portal)
- Creating an open access to their healthcare provider (patient portals, electronic communication etc.)
- Creating self-management goals for certain conditions such diabetes (for example patient agrees to walk for 30 minutes/5 days a week)
- Discussing various treatment options
- Allowing the patient and the family, in essence, be a part of the health team
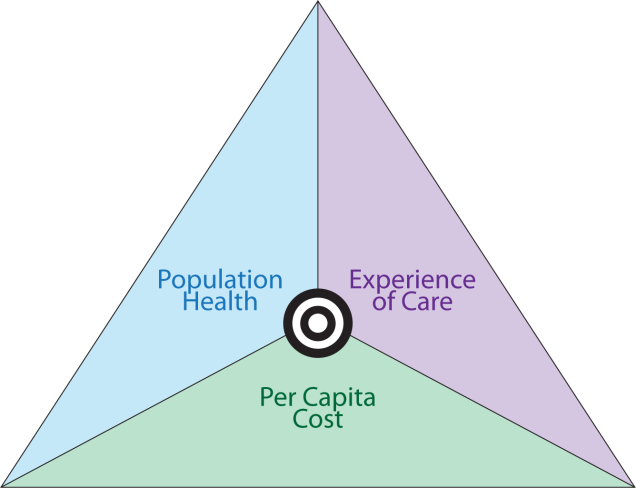
Improved patient engagement, in theory, could lead to improved outcomes, decreased resource utilization and improved patient satisfaction.
Figure 3: Triple Aim model from the Institute for Healthcare Improvement7
The Blue Button is one such governmental initiative that will give patients increased access to their personal health information.
Figure 4: www.healthit.gov/bluebutton

The case for improving the EHR end-user experience to improve patient engagement.
The good physician treats the disease; the great physician treats the patient who has the disease.
-Sir William Osler ( 1859-1919, one of the founders of Johns Hopkins Hospital)
Healthcare workers including physicians are being asked to do more with less. The impact of EHRs on their workflows has been tremendous. Increasing patient engagement would further disrupt their workflow. Currently healthcare is mostly encounter driven. Patient care is evolving from being episodic to being continuous Healthcare workers, especially clinicians, will be expected to be always ‘on’. They will become responsible to react to patient data 24/7 not just when the patient’s status changes. For example, in past the clinician could wait to respond to a result if it was not abnormal or critical. With real-time access, patient can now see the result via a portal and securely message the provider with questions. For patient engagement to cause least disruption and stress to healthcare clinicians and workers:
- EHR vendors will need to pay more attention to the end-user experience. Both the government and the clients will need to leverage this.
- EHRs will need to evolve to become efficient tools.
- Healthcare organizations will need to think (and rethink) risks of patient privacy vs. benefits increased/improved EHR access to healthcare workers.
- Patients and staff will need to be counselled on what constitutes appropriate response times.
- Information Technology leaders such as CIOs and CMIOs will need to pay more attention to the end-user satisfaction.
- There are very good physicians and staff in all organizations who struggle with some or all aspects of the EHR. To retain such team members, healthcare organizations will need to devout more resources to train and support.
- Clinician reimbursements will need to move away from fee for service (episodic) towards fee for quality (value based continuum).
The focus should always be the patient. Patient satisfaction cannot be achieved without provider satisfaction.
References
- http://blog.softwareadvice.com/articles/medical/ehr-timeline-113/
- http://www.apapracticecentral.org/advocacy/technology/hitech-act.aspx
- http://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/Meaningful_Use.html
- http://www.acponline.org/pressroom/ehrs_survey.htm
- http://www.idc.com/getdoc.jsp?containerId=HI244027
- http://www.hrsa.gov/healthit/toolbox/HealthITAdoptiontoolbox/MeaningfulUse/intro2meaningfuluseandpatientandfamily.html
- http://www.ihi.org/engage/initiatives/TripleAim/Pages/default.aspx
