Summer 2014 - Roving Reporter
A Roving Reporter’s Review of the 6th Annual Clinical Informatics Summit - May 2, 2014
by Karen Keating
Necessity: the Mother of Invention
Apt words spoken by Bill Childs in his keynote address to the 6th Annual Clinical Informatics Summit on May 2nd.
Before Bill was awarded a Lifetime Achievement Award for his decades of contributions to HIT, he reflected on where we’ve come from, the early days of 1968 when Medicare/Medicaid were established. When engineers literally ‘built’ keyboards, monitors and DRGs were new. Leading up to now, when we need ‘Star Trek’ medicine – i.e. smart systems that do more and help us innovate costs out of the delivery process. As an early pioneer in electronic records, Bill was part of the team that wrote an EMR for Lockheed, which they installed at El Camino Hospital saving $1M dollars the first year.
Fast forward… Change has become the new normal – new systems and technology, new medical procedures, diagnostic tools and therapies, government introduced change and organizational change to adapt to the pressing demands. This is but a partial list of the changes we face on many fronts.
One thing is certain, however, the escalating cost of healthcare cannot continue. As it approaches 20% of GDP, providers and organizations explore numerous strategies to leverage technology and shift care to less costly settings. From the acute hospital to the clinic to the home and out into wellness programs in the community preventing the need for care and promoting health across society.
The over-65 population is forecast to reach 72 million by 2030, a mere 15+ years from now. While demand for services will surely increase, reimbursement will struggle to keep up. With more new patients brought into the system by the Affordable Care Act (ACA), it quickly becomes apparent that efficiency, innovation and prevention are paramount.
This era of specialization may need to be put on life support as it’s simply not scalable to add people, increase services and maintain a high degree of specialization. Cost is not sustainable and human resources may not be available. Further, when stringing together many sub-specialists, there is a need for ‘knowledge couplers’ to ensure continuity. Reducing human touch-points can potentially improve both quality and efficiency.
Our challenge as health professionals is to solve this difficult equation quickly while protecting quality. Presentations at the April HIT Conference and the May Informatics Summit showcased the tremendous creativity and dedication of our members.
You can tune in to our YouTube Channel to view the presentations: https://www.youtube.com/user/socalhimss
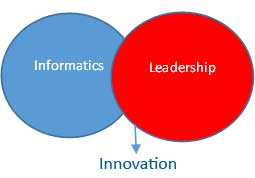
The Vital Intersection of Informatics & Leadership: Subspecialty referrals in the LA County Department of Health Services - Paul Fu Jr., MD, Harbor-UCLA Medical Center
To set the stage, Dr. Fu began with slides on Human Centered Design and presented the value of storytelling as a useful tool to manage change. Then he reviewed the DHS initiative to correct problems with the physician referral process, which involved a system solution combined with redesigning processes and workflow.
Before the referral process was re-vamped, patients experienced long wait times. In 2011, it could take between 86 to 225 days for a referral appointment. No-show rates were high and there was poor coordination and between Primary and Community physicians. Overall there was high variability in the care processes between clinics.
With grant funding and strong leadership, intent on using IT to drive a solution, the team deployed an eReferral system by Siemens. They documented the chaotic and unpredictable ‘old’ state and rolled out a system-driven solution with redesigned workflow to 23 specialty clinics.
The results were dramatic. In 2014, the wait time ranged from 44-71 days. There was improved coordination and communication between doctors and case closure rates increased. Most important, patients received care more quickly. Plans include finishing the rollout to surgical, pulmonary, dental and vascular clinics.
Dr. Fu and the DHS team’s success demonstrate the value of optimizing systems and human workflow. This is the promise of innovation – take good ideas and improve on them in your own environment.
Technology Innovations in Acute Care: What Palomar Medical Center is Doing for Patient Safety
Breana Feistel, RN, Palomar Health
Goals: Decrease the noise level for patients and minimize alarm fatigue.
Challenges: Moving to a new building. Ambulatory patients on telemetry lose WIFI signal in the garden.
An advisory board reviewed the clinical factors and technical environment to make decisions on the project strategy. What follows are findings that may benefit your projects. Work at Palomar continues as they audit call volume and workflow and adjust procedures to further reduce noise and interruptions in patient areas.
Start small and leverage Lessons Learned in subsequent phases.
Roles change when new care models or technology are introduced. Plan for training.
After initial rollout, 35 alerts in multi-disciplinary rooms were deactivated.
Turning off SPO2 reduced 20 thousand alarms per day!
Review the default alarm settings on monitors
Improving response time can prevent escalated calls that adds to the noise level.
Standardize and fine-tune the new alarm & alert technology.
Subject matter experts (SME’s) and Leaders are key to adoption. They have an important role to play.
They can help decide what alarms and alerts are actionable.
SME’s can develop materials, train nurses and provide Go Live support and coaching.
Leaders on the units, engaged with staff and addressing issues, improves morale and adoption.
Legislative Roundtable – Members of the CA Assembly and Federal Government
Sri Bharadwaj and John Risk encourage all of us to review the Advocacy & Policy page of our website. Making HIMSS expertise available to legislators can contribute to more informed decisions.
http://www.himss-socal.org/advocacy1/advocacy1.html
Big Data in Healthcare
Charles Boicey, MS, RN-BC, Stony Brook Medicine
Homework was assigned before Charles reviewed how he gleans nuggets of information from vast amounts of data. He suggested viewing Jacob Barnett on UTube, a brilliant young astrophysicist with an important message. He also recommended learning the new technology used by Facebook & Twitter.
Big Data in Healthcare: The SoCal Experience
Kim Jackson, BA, St. Joseph Health Systems
What’s the difference between an Electronic Medical Record (EMR) and an Enterprise Data Warehouse (EDW)?
EMR data is ‘Live’ and updated as close to real time as possible. Data from source systems is transactional and intended to support clinicians providing care. EMRs are not built to process extremely high-volume or high-velocity data or perform complex operations, such as anomaly detection.
An EDW has a latency factor – i.e. data is retrospective. A wider variety of data serves clinical, operational, quality and research purposes. It originates from the EMR and other sources. It’s an ideal platform for modeling advanced or predictive analytics.
Big Data can satisfy various information consumers: clinicians, researchers, decision-makers. It can provide a holistic view of the patient. It can be used to fulfill many broad objectives – population health, regulatory compliance, program development, quality and process improvement to name a few.
Big Data requires special skills. Data Governance is critical. Data Stewards and Knowledge Workers must manage data definitions to ensure that information is accurately interpreted. Security, governance and training contribute to a well-managed system.
In a new healthcare paradigm, there is a need for predictive & prescriptive analytics. When Big Data is accurate, standardized and complete, it can be transformed into actionable information, knowledge and wisdom.
Health Information Exchange / Population Management in 180 Days
Jamie Anand, MSN, RN, UC Irvine Health
HIEs & Data Exchanges
Let’s start with defining Health Information Exchanges (HIE) and Health Data Exchanges.
Health Information Exchange (HIE) is the mobilization of healthcare information electronically across organizations within a region, community or hospital system.
Health Data Exchange (Interoperability) is the ability of different systems and software applications to communicate, exchange data, and use the information that has been exchanged.
How does an HIE align with clinical and organizational goals? HIEs can make more complete patient information available to caregivers, which can improve safety, quality and reduce duplication, thereby reducing cost. They can be used to manage the growth and evolution of clinical programs. Active use of aggregated patient data can be used for programs that improve community health.
Data exchange (interoperability), provides additional benefits, chiefly expanded access to services for patients. When a patient’s information is more readily available to clinicians, they have a more complete from which to make decisions on the plan of care. In order to fully achieve the goals of Accountable Care Organizations (ACOs) and Population Health we’ll need operational HIEs nationwide.
UC Irvine uses their DB Motion HIE to:
integrate with OCPRIO, which sends data to National Health eWay
Connect to California Registries – Gateways for immunization data and reportable diseases
Connect with Partners HIE – to – HIE
Connect patients to health resources like the California Smoker’s Helpline
In the future, after technology updates, connect with other UC Medical Centers
Portals
Patients are gaining interest in managing their health using electronic tools and portals can further this trend by providing online access to health records. This access has been shown to stimulate patient activation. The UCI Portal ‘Follow My Health’ was selected because of its ease of use. Visits at multiple hospitals can be seen in one portal. It can be used on an iPad or a smart phone and it can translate information into Spanish.
What do patients want from a Health Portal? Beyond access to web-based health records, forms and the ability to pay online, patients want to obtain a physician consult via email and receive email reminders of appointments.
As more organizations connect to HIEs, exchange information and install patient portals, the web of health information available for providers and patients will continue to be enriched. Exciting times ahead!
Karen Keating, Roving Reporter, is co-chair of HIMSS So Cal Marketing Committee and a consulting Project Manager (PMP). You can contact her at kkeating1111@gmail.com.
